Supporting Muslim patients in consultations – a guide for healthcare professionals
This guide helps healthcare professionals (HCPs) (e.g. pharmacists, GPs) hold informed, respectful, and person-centred discussions with Muslim patients, carers, and families about medicines and halal considerations.
It does not direct prescribing or treatment decisions but highlights key considerations that may arise in consultations or from patient queries.
Key considerations
1. Ingredients and excipients
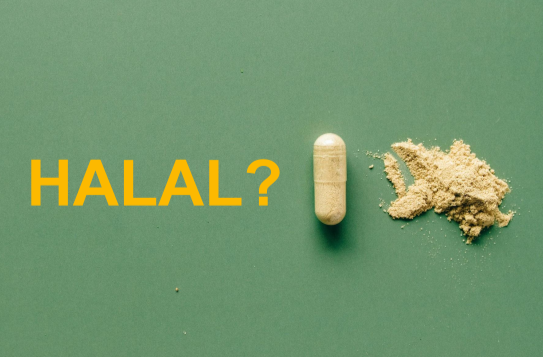
- Some medicines contain ingredients and/or excipients that may be a concern for practising Muslims (e.g. gelatine, ethanol), it is important to know what these may be
- You may be asked to help check if certain ingredients and/or excipients are present in medicine(s) and their source, as they may be from haram (prohibited) sources.
- Further clarification of the source and processing during manufacturing is often needed before confirming their halal status
- You may be asked to help patients gather further information about ingredients and/or excipients in medicines and classify them to determine if a medicine is suitable for a halal diet.
🔗 Useful links
- HalalMed ‘Simple checklist‘ – to check which ingredients and/or excipients may be a concern for practising Muslims
- HalalMed ‘How to check if a medicine contains ingredients and/or excipients from haram sources‘ – to check if a medicine contains ingredients and/or excipients from haram sources
- HalalMed ‘Ingredients and excipients in medicines’ – detailed resources to find out if an ingredient or excipient is halal or haram
- HalalMed ‘Reason codes’ and supporting resource on ‘How we classify medicines based on ingredients and excipients’ – to find out how we classify ingredients, excipients and halal status.
2. Person-centred discussions and gathering information
- Encourage and initiate person-centred discussions about concerns, expectations or personal beliefs
- Gather information by asking open questions
- Ask if the patient has specific religious needs and what these are
- Clarify if they wish to avoid certain ingredients and/or excipients and what these are.
- Explore the patient’s personal values and beliefs – religious practice and interpretation may vary between individuals, so avoid making assumptions
- Some patients may wish to avoid certain ingredients and/or excipients entirely, whereas others may wish to do so in specific circumstances only; therefore, it is important to ask and clarify each patient’s individual preferences
- Levels of religious observance and personal conviction may also differ between individuals; therefore, it is important to ask and clarify each patient’s individual preferences.
🔗 Useful resources
- HalalMed ‘Conditions for permitting an impermissible medicine‘
- HalalMed ‘External resources for healthcare professionals‘ – further useful signposting for HCPs
3. Explaining findings
- Share whether the medicine contains potentially problematic ingredients and/or excipients
- If unclear, explain that more information from the pharmaceutical companies may be needed.
🔗 Useful resources
- HalalMed email template – to request information from pharmaceutical companies.
4. Exploring alternatives
Patients may ask about exploring possible options:
- 💊Alternative formulations (where available) – e.g. formulations that do not contain a concerning ingredient and/or excipient
- 🌿Alternative treatments – if clinically suitable and guided by national or local prescribing guidelines.
⚠️ Always use clinical judgement to consider clinical appropriateness, patient safety, availability, and guideline recommendations before suggesting alternatives.
🔗 Useful resources
- Specialist Pharmacy Service (SPS) resource on ‘Searching for presence or absence of an excipient in medicines‘ – to search for medicines that do not contain certain ingredients and/or excipients
- The NHS Business Services Authority (NHS BSA) ‘NHS dictionary of medicines and devices (dm+d) browser‘ – to search for alternative formulations
- The National Institute for Health and Care Excellence (NICE) ‘British National Formulary (BNF)‘ – to search for alternative formulations.
5. Explaining limitations
Patients may ask about exploring possible options:
- There may be situations where:
- No halal alternative is available
- You cannot prescribe or supply a halal alternative.
- Be clear and transparent when this is the case and explain the limitations on prescribing or supplying a medicine
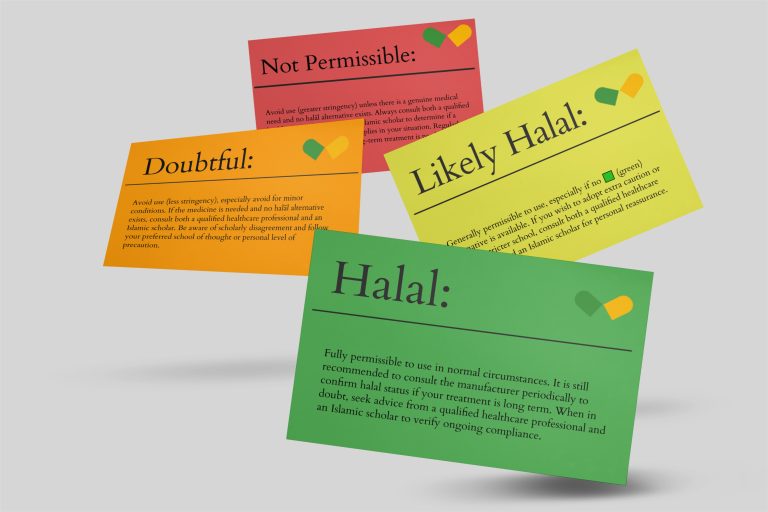
- It is important to remember that even if a medicine contains ingredients and/or excipients from haram sources, it does not always mean it is prohibited to take or use. In certain circumstances, medicines containing ingredients and/or excipients from haram sources may still be permissible
- You may find it helpful to explain the guidelines around ‘hardship begets facility’ (al-mashaqqa tajlib at-taysir) – meaning that when practising a religious ruling becomes overly burdensome or causes genuine hardship, leniency (rukhsah) may be applied to bring ease, particularly in cases of necessity or significant need. This principle also extends to HCPs when prescribing or supplying medicines under such circumstances
👉 You can find out more about hardship begets facility here.
- You may find it helpful to explain the guidelines around ‘hardship begets facility’ (al-mashaqqa tajlib at-taysir) – meaning that when practising a religious ruling becomes overly burdensome or causes genuine hardship, leniency (rukhsah) may be applied to bring ease, particularly in cases of necessity or significant need. This principle also extends to HCPs when prescribing or supplying medicines under such circumstances
🔗 Useful resources
- HalalMed ‘What to do if a medicine contains ingredients and/or excipients from haram sources‘ – to learn when it may be acceptable for a Muslim patient to use a medicine containing ingredients and/or excipients from haram sources (see section on Hardship begets facility) and limitations on prescribing alternatives (see section on Limitations on prescribing an alternative halal medicine).
- HalalMed ‘Conditions for permitting an impermissible medicine‘ – to find out about the five conditions.
6. Respect and shared decision-making
Patients may ask about exploring possible options:
- Respect the patient’s beliefs
- Support them in making informed decisions about their treatment and medicines that balances clinical appropriateness with their religious values and beliefs
- Ensure they feel listened to, respected, and supported in their decisions
- Consider health literacy of the patient – by providing information in small and easy-to-understand parts, checking for understanding by asking open questions and asking the patient to explain back to you what they understood in their own words, and clarifying if needed to correct misunderstandings
- Agree actions and next steps – document any useful or necessary information in the patient’s record.
⚠️ Important information for patients
- Always take or use your medicine(s) exactly as directed or prescribed by your healthcare professional (HCP), such as your doctor or pharmacist
- Do not stop, delay, change or alter the way you take or use your medicine(s) without first discussing it with the HCP who prescribed or supplied it to you
- Always consult your HCP if you have any questions or before making any decisions about your treatment
- For Islamic guidance, seek advice from your local Imam or a trusted Islamic scholar – ideally someone with relevant knowledge and expertise in the fiqh (Islamic rulings) of medicines
- Use the information gathered to make an informed decision together with your HCP and, if needed, your local Imam or trusted Islamic scholar
Disclaimer
- This resource is for educational purposes only. It does not constitute clinical, medical, or professional healthcare advice and should not replace individual clinical judgement or qualified religious guidance
- Always consult your doctor, pharmacist, or other healthcare professional regarding your own medical conditions or for advice on treatment options
- Healthcare professionals remain fully responsible and accountable for decisions made within their own scope of practice.
Further resources
- Ingredients and excipients in medicines – detailed resources on ingredients and excipients commonly used in medicines which may raise concerns for the Muslim community
- Checklist of ingredients and excipients – a quick checklist of ingredients and excipients commonly used in medicines which may raise concerns for the Muslim community
- How to check if a medicine contains ingredients and/or excipients from haram sources – explains how to check medicines for ingredients and excipients that may be an issue in Islam, and what to do next
- What to do if a medicine contains ingredients and/or excipients from haram sources – find out when it may still be acceptable to use medicines containing ingredients and/or excipients from haram sources, and why a halal alternative may not always be available
- Email template – to request clarification from pharmaceutical companies
- Reason codes: how we apply our classifications to real medicines – our classification codes for ingredients and excipients
- How we classify medicines based on ingredients and excipients – supporting guide for reason codes
- External resources – for healthcare professionals.